Statins- Lifesavers or the biggest pharmaceutical fraud ever?
This is the second part of the series I wrote about our current dietary and medical recommendations to prevent heart disease. The first part explored the dietary component and some of the common misconceptions regarding cholesterol and saturated fat. This article explores the use of statin therapy and its many implications. This is very important to me personally since a very large percentage of my clients are over 60 and on statin medications currently. My clients are like my family and their well being is what drives me. Unfortunately in this western medicine based society we are very quick to take pills as an answer rather than addressing the underlying cause. High cholesterol- take a pill, Feeling unhappy?- there are plenty of pills for that including SSRI's. Who needs to address the physical and mental reasons your feeling depressed. Elevated blood sugar? Take this and become dependent on it to regulate your glucose. Have a muscle or headache? There is a seemingly endless amount of pain meds to choose from. Its our go to solution. Just give me a pill. We are a medicated society and the ramifications are long reaching. /end rant. Ok lets see if we can get a better understanding of statins and possibly get them off the list of unnecessary medications. The main questions addressed in this part are:
- What are statins and how do they work?
- What are potential adverse affects of taking statin medication?
- What are our current and past guidelines based on for prescribing statin therapy?
- Are statins effective?
- Has Big Pharma corporate interests influenced our current drug policy?
In my previous article I discussed how despite some studies showing a correlation between serum cholesterol levels, LDL-c in particular, there was not enough evidence to label it as causal with CHD since the correlation did not appear among all populations and there were even more studies showing the exact opposite. Yet millions of Americans are taking LDL lowering drugs in hopes of reducing risk of CHD. So are statins safe and effective? First we should try to delve a little deeper into what exactly a statin is.
wow that is quite a complex process that is being disrupted
A statin is a HMG-CoA reductase inhibitor. This enzyme regulates the production of melavonate which is a precursor to producing cholesterol. Melvonate is also vital in the process of cell regeneration aka life. Its inhibits production of CoQ10 which is vital for cell energy, in fact its a 20+ step process from HMG-CoA reductase to the production of cholesterol so there are many biological functions in this complex process that are being inhibited as well. The inability to produce cholesterol through this process leads our LDL receptors to take up more LDL in the blood to make up for the lack of endogenous cholesterol. Thus we have a large drop in LDL and very happy pharmaceutical companies. So does this drop in LDL lead us to being a healthier person with a longer life? Continuing to explore the mechanisms of statin therapy will paint a clearer picture.
Most people who take statins know that it lowers their LDL-c. That's about it though. Since most people think of LDL-c cholesterol as bad they see this as a positive thing. But remember as we covered earlier there is no good or bad cholesterol, cholesterol is the same no patter what kind of particle is transporting it. Cholesterol is not bad, LDL-c is not even bad. Its only bad when a LDL-p gets stuck in the endothelial wall and oxidizes. Also there are a number of factors that contribute to this possibility: weak arteries, high ldl-p, higher propensity of small dense ldl, oxidizing factors... its a very multifaceted condition. Statins work by reducing the concentration of LDL in the blood so a by product of this is lower cholesterol. Unfortunately cholesterol isn't the only thing LDL transports to our cells, it also transports fats, vitamin D, and fat-soluble anti-oxidants to all of our bodies tissues. Since the liver synthesizes much of the cholesterol supply to the cells, statin therapy greatly impacts the liver, resulting in a sharp reduction in the amount of cholesterol it can synthesize. A direct consequence is that the liver is severely impaired in its ability to convert fructose to fat, because it has no way to safely package up the fat for transport without cholesterol.(1) Fructose builds up in the blood stream, causing damage to serum proteins and an increase in blood sugar levels. It's clear that a drug that has this profound of an effect on an individuals biochemistry is going to be linked to some serious side effects.
Side effects of statins
From Lipitor's website they warn of the following possible side effects:
- Muscle damage (largely because of CoQ10 depletion)
- Kidney damage
- Liver damage
- Diarrhea
- Muscle and joint pain
- Alterations in some laboratory blood tests.. (the FDA revised guidelines in 2012 saying all statins must present the possible side effect of diabetes or elevated blood sugar. In the last year and a half the pharmaceutical companies have been able to get that label taken off by making the above statement. The FDA lightened its stance, after reviewing evidence from both Merck and Phizer(and receiving more funding most likely)
- Tiredness
- Tendon problems
- Memory loss
- Confusion
These are all the side effects that the FDA requires to be on statins here in the USA... but we are missing a big one, CoQ10 depletion which can lead to impaired cardiac functioning in patients with congestive heart failure. (Funny thing is this is on the labeling in Canada but in America the FDA does not require this warning. Maybe us Americans are so boss we don't need CoQ10) There are many other reported adverse affects out there. Its important to note that the warnings for memory loss, liver damage, increased blood sugar, development of type 2 diabetes, and muscle injury weren't put into place until 25 years after they were first being used. These didn't just develop overnight, it took years worth of observational studies before that conclusion could be made. The American public is currently unknowingly participating in a long term study on how interrupting and stopping one of our most basic biological funtions from occuring (production of cholesterol and the whole melvonate pathway) is going to effect the lifespan and quality of life when using statins long term. How could something get approved for long term use, for those not even high risk no less, without any long term studies? Follow the money. The following are more side effects that are a result of statins. Since these ones are not on the label I've provided studies presenting the evidence. This is largely dose dependent and side effects increase with more statins.
- Neurological issues such as europathy, parasthesia and neuralgia, and lower risk but more debilitating neurological diseases, ALS and Parkinson's disease.(2) Its thought that myelin sheath (which transmits impulses from the brain) is impaired from faulty cholesterol delivering mechanisms caused by statin therapy. This could lead to a "faulty connection" neurologically speaking.
- Rhabdomyolysis(3) This is caused when the degeneration of muscle tissue leads to by-products being released in the bloodstream. The statin Baycor (from Bayer) was removed from the market in 2002 for being linked to rhabdomyolysis. Muscle-related adverse events due to medicine occur more often in real life than they do in clinical trials because high risk patients are typically not included in a controlled setting.
- Cataracts(4)
- Diabetes type 2(5)(6) especially in post-menapausal women(7) and those taking higher doses of statins(8)
- More exercise related muscle injury(9)
- Sexual dysfunction in men(10)
- Increased chance of prostate cancer in men(11)
- Increased chance of breast cancer in women. The 1996 statin CARE study would have widely published its mostly favorable results except that in women there were 12x the cases of breast cancer in those taking pravastatin.
Nearly 75% of new statin users will discontinue their treatment within this first year- THe most common reason by far is negative side effects
With all these potential negative side effects statins must be extremely effective to be worth the risk right? Lets take a look at some of the largest studies involving statins to draw some conclusions.
The studies
John Gormans work identified that high HDL was benefical and high LDL was often correlated with CHD. The Framingham study had shown LDL-c it to be a risk factor in middle aged men. These are the two main reasons LDL became the target for drug therapy. How did we come to our current views regarding statin therapy and how did statins go from being prescribed to the 1 in 500 who have the genetic default familial hypercholestermia to 1 in 4 Americans over 45 currently?
- 1973- Joseph Goldstein releases the results of an investigation into familial hypercholesteremia: this was a landmark study because it was the first time a specific receptor of cholesterol had been found. This would spur a decade of research to find a drug that could be used to artificially lower cholesterol- even though there had been no definitive study proving blood cholesterol had a causal relationship with heart disease
- 1977- The first statin, Compactin, is developed by Akira Endo to treat those who have the genetic defect familial hypercholesteremia which causes their LDL receptors to not be fully functional
- 1978- First patient with familial hypercholesterimia is given Compactin and LDL levels are lowered about 100mg/dl.
- 1979- Merck devlops its own statin, Lovastatin
- 1980- Compactin is discontinued due to high rates of cancer in dogs when given high doses and Merck halts its studies on Lovastatin
- 1984- LRC-CPPT(12): used as proof that lowering LDL lowers CHD. All participants were men diagnosed with primary hypercholesterolemia which only 1 in 500 people in the general population have. Yet the results for this specific group of people with a specific genetic defect was extrapolated to the general public. As mentioned earlier there was a small drop in chances of having a non-fatal myocardial infarction in the group that was taking the cholesterol lowering drug cholestyramine but no difference in overall mortality. A 19% reduction of risk of CHD related death or event was reported. Its important to be aware of how easy it is to paint a picture using risk in relative terms instead of absolute terms. Any reporting of risk in a study financed by big pharma will always be relative and not absolute, so long as its favorable. What this relative 19% reduction in cardiac events really means is that there was an incidence of 8.6% in the control group and 7.0% in the experimental drug group.(Relative risk=(R1-R2)/R1) So in reality its a 1.6% drop in absolute risk. (Absolute risk=R1-R2) This is used as evidence for the need to further develop statins since they were thought to be better tolerated and more likely to be used compliantly as an easy pill. (Cholestyramine was resin in a packet you had to ingest) Funded by The National Institute of Health.
- 1987-FDA Reviews and revises National Institutes of Health protocols for lowering cholesterol levels with lovastatin from Merck. Based off a few small short term studies it becomes first statin approved for use by FDA in record time, 9 months. This approval is based off proof lowering LDL levels through the statin, not through any mortality or cardiac related endpoints. The loose correlation that had been seen in some studies between LDL-c and incidents of heart disease is used as justification despite the fact that their were many other studies showing no correlation at all, especially in women and the elderly.
- 1991- Expanded Clinical Evaluation of Lovastatin study results(13): This was the first large statin therapy study containing over 8000 patients with moderate hypocholesteremia. While cholseterol levels were lowered using Lovastatin all cause mortality increased. This was sponsored by Merck and other than the first year it was published, no report over the last 20 years has included a figure for all-cause mortality or mortality endpoints from heart disease. The official response from Merck has been that the trial was not designed to measure the clinical outcome, only to test whether the drug was tolerable and did not produce any serious side effects. Im quite sure if the clinical outcome were favorable we would be hearing about it.
- 1994- Scandinavian Simvastatin Survival Study(14): This study ushered in a large amount of new statin users for secondary care. Prior to the 4S study statins were mainly being used in people with genetic defects that interefere with ability to clear LDL-c from the blood, and a few men who were very high risk and already had severe hypercholesteremia. This was the first large study investigating the effectiveness of statins as a form of secondary prevention from those who had already had a CHD realated event. It showed a decrease in death from CHD and a lower all cause mortality as well in men under 70. Study was discontinued halfway through, and there were slightly more deaths in women taking statins. I believe the primary end points may not have reached statistical significance if the study had been followed through for the intended duration. Statins negative effects often appear years after the initial positive ones and I think its quite likely cancer and other causes of mortality would have increased as they have in similar studies. This was sponsored by the pharmaceutical company Merck.
- 1995- The West of Scotland Coronary Prevention Study(15): This is considered the first very positive case for men to be using a statin for primary care who are high risk of CHD. Those taking the statin had a 1.9% risk reduction in cardiac events and a .9% reduction in all cause mortality. Of course these were presented as relative risk reductions of 29% and 22% respectively. The average bmi of the participants was 26 and the participants drank and smoked more than the average male. So within a year and a half statins went from being perscribed almost solely to those with specific birth defects to being used for secondary care for both men and women and primary care for high risk men. This greatly increased the market for this drug
- 1996- The Cholesterol and Recurrent Events(16): Another study on secondary prevention for those who have exeperienced myocardial infarction. The difference between this and the early 4S is that although they had recently experienced myocardial infarction these paitents had normal cholesterol and LDL levels. Total cholesterol and LDL-C were lowered as were cardiac events, no significant difference on CHD or all cause mortality. 1 woman developed breast cancer in the placebo group and 12 developed it in the statin group.
- 1998- AFCAPS/TexCAPS(17): This was designed to test if moderate dose primary care statin therapy would reduce CHD in those who were low risk. It involved over 5500 men and almost 1000 women. It reduced the chance of having a first cardiac episode but more total deaths than in the placebo group. Funded by Merck. This ushered in a new group of people for primary care who weren't at a high risk , still mostly men at this point, to statin therapy since it reported the significant reduction in coronary events but did not really publicize the non signifcant increase in deaths. Since these are low risk people the risk of an event is low to begin so the absolute decrease in risk is quite small yet you are still implored to take biochemistry altering drugs.
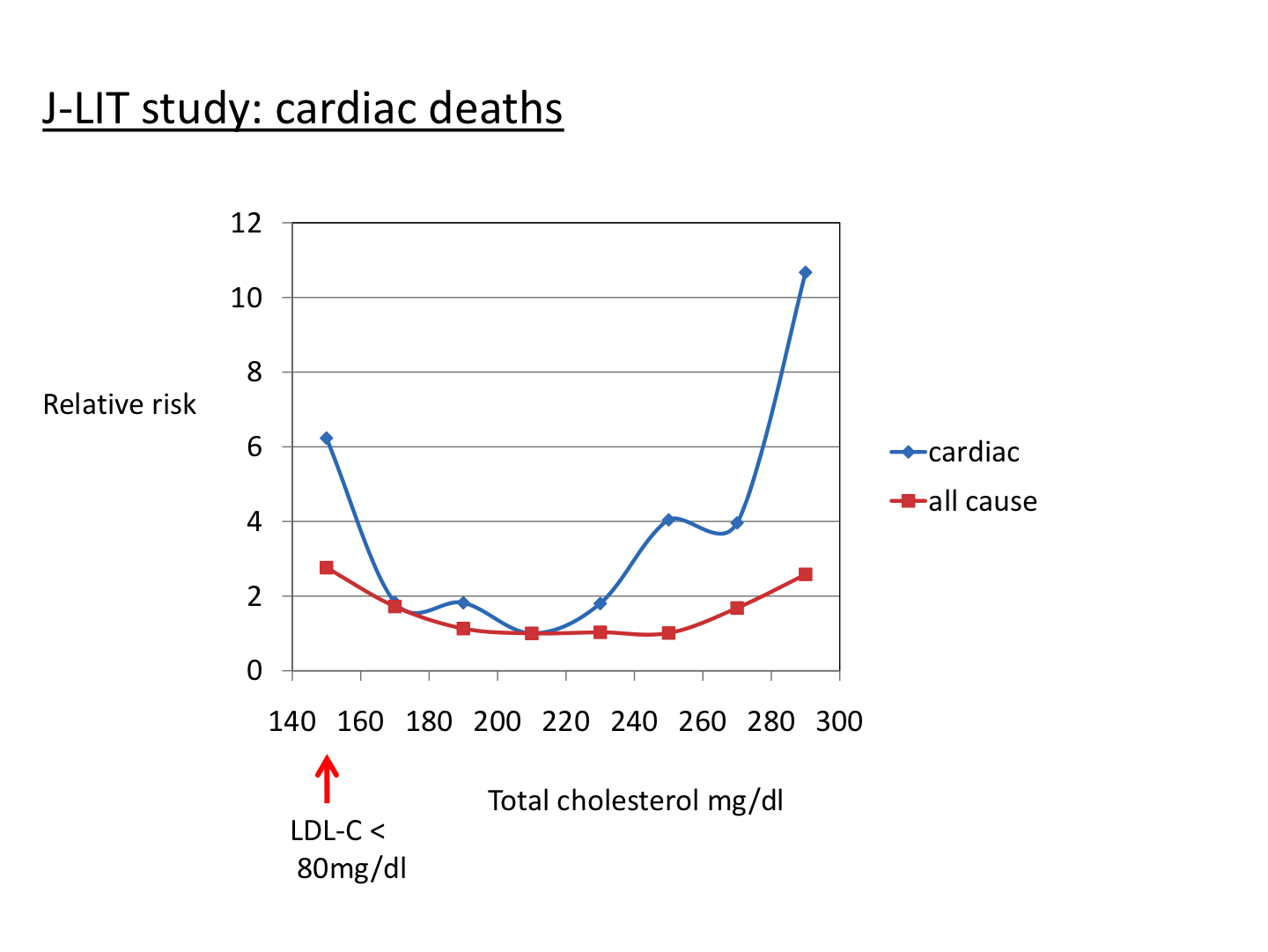
- 2002- Japan Lipid Intervential Trial(18): Primary prevention study that involved over 45,000 patients over 6 years, 2/3rds were women. There was no placebo group just 2 groups using different doses of Simvistatin. Those on the higher dosage lowered LDL-c more but also experienced high cardiac and overall mortality rates. This is one of the many cases where LDL and CHD do not correlate and those with the lowest LDL and total cholesterol had the highest rates of death. Even though those with extremely high cholesterol levels had more cardiac related deaths absolute mortality was almost identical as those with the lowest.
- 2002-The Prospective Study of Pravastatin in the Elderly at Risk(19): this study involved 5000+ patients over the age of 70 who either had pre-existing vascular disease or very high risk. There were signifcantly fewer CHD related deaths, but no difference in total mortality due to a large increase in deaths from cancer in the experimental group, despite having much less smokers. Sponsored by pharmaceutical company Bristol-Myers Squibb. Since CHD is the leading cause of death in the elderly and the statins reduced CHD mortality it ushered in a large group of seniors who had previously not seen any studies proving benefits.
- 2003-Anglo-Scandinavian Cardiac Outcomes Trial--Lipid Lowering Arm(20): Large study with high risk patients who have not yet developed CHD aged 40-79. All participants had hypertension and average BMI was 29. This was similar in design to the WOSCOPS trial and provided similar results in men. The statins lowered CHD related events and deaths slightly. It was stopped 2 years early and was financed by Pfizer.
- 2004- Treating New Targets Study(21): 5 year study with over 10,000 people who have stable coronary artery disease comparing 10mg dose of lipitor to 80mg dose. Much lower LDL cholesterol was found in those taking the maximum dose and there were significantly fewer CHD related deaths. Overall mortality actually increased slightly however. This study was sponsored by Pfizer. Average dose for Americans at this time was 10-40mg for very high risk patients. This study did not usher in a new demographic as others have but it did convince the public and the medical community that more statins are better, increasing profits further significantly again. Many high risk patients had their dosage doubled since their were low reported sides and non-significant change in mortality while significantly less CHD deaths
- 2004- PROVE IT-TIMI(22): Study involved over 4,000 people who had recently experiened a cardiac event. One group was given a statin at 40mg an the other was given 80mg to determine the benefits and risks of intensive statin therapy. The higher statin group experienced lower rates of CHD and overall mortality. The more intensive therapy group also had more participants quit due to myopathy (muscle pain.) Sponsored by the makers of one of the statins, and multiple authors have major conflicts of interest since many either serve as a consultant for one of the pharmacy companies involved or have recieved funding.
- 2004- The U.S. government's National Cholesterol Education Program panel changed guidlines for statin therapy candidates to include anyone considered at moderate to high risk who does not have LDL under 100mg/dl or even 70mg/dl for the very high risk. These levels are very tough to achieve without use of statins and this increased the treatment base dramatically. 8 of the 9 members of the council received funding in the form of grants, speaking fees, and consulting fees from multiple companies that manufacture statins.
- 2008- The Jupiter Trial(23): This is used as justification of use of statins for primary prevention for all people not currently high risk for CHD but had above average levels of C-Reactive Protein which is an indicator of inflammation. This included the elderly and women who had previously not seen many benefits from statin therapy for primary prevention. All participants had LDL levels under 130mg/dl which was below the threshold for statin therapy at the time. This study found statistically significant drops in heart attacks, stroke, and all cause mortality for those taking the statin. It was the first to show a positive benefit with the elderly and woman, and to also significantly decrease all cause mortality. The only negative take away I could really find was higher rates of diabetes in the statin group. There was a 25% increase in relative risk of devloping diabetes. Had the study ran the intended time, the prolonged time having elevated blood sugar levels may have balanced things out less in favor of the statins. This was sponsored by the drug company Astra Zeneca who collected the trial data and monitored study sites. There were multiple conflicts of interest and the main author of the original study owns the patent to the test being used to identify CRP levels.
- 2010- Cholesterol Lowering, Cardiovascular Diseases, and the Rosuvastatin-JUPITER Controversy(24): critical paper from the Journal of American Medicine claiming the JUPITER study is flawed and did not support the use of statins for primary prevention. Their final conclusion: "The results of the (Jupiter) trial do not support the use of statin treatment for primary prevention of cardiovascular diseases and raise troubling questions concerning the role of commercial sponsors."
- 2013- American Heart Association publishes The New Guideline for Management of Blood Cholesterol. The new treatment guidelines focus on risk factors instead of just cholesterol and double the number of Americans viewed as candidates for statin therapy. 6 of the 15 panel members, including the co-chair, had financial conflicts of interest and were receiving some form of funding from Big Pharma.
- 2013- Comparative effectiveness of exercise and drug interventions on mortality outcomes(25) a metanalysis from the British Medical Journal involving 305 randomized trials and almost 340,000 people found no benefit to using either statins or beta blockers over exercise to lower risk of cardiac events.
- 2013-The Ugly Side of Statins. Systemic Appraisal of the Contemporary Un-Known Unknowns(26): a systematic review of major statin studies was conducted by independent researches and published in the Open Journal of Endocrine and Metabolic Diseases. They analyzed risks associated with primary care and found for every 10,000 people taking a statin, there were:
- 307 extra patients with cataracts
- 23 additional patients with acute kidney failure
- 74 extra patients with liver dysfunction
The landmark review revealed "a categorical lack of clinical evidence to support the use of statin therapy in primary prevention." They also found that statins actually increase cardiovascular risk in women, the young and people with diabetes. The review also showed that statin therapy increased:
- Muscle fatigabilty by 30% with more than 11% incidence of rhabdomyolysis (a life-threatening muscle condition) at high doses
- Coronary artery and aortic calcification
- Erectile dysfunction, which is 10 times more common in young men taking the lowest dose of statin.
- Diabetes
- Cancer
How effective are statins?
If we were to gauge the effectiveness of statins based on whether they significantly lower LDL-c they would no doubt be considered effective. But we are primarily concerned with the two end points of death from coronary heart disease and all-cause mortality. We will also pay attention to rates of myocardial infarction because there are a wide array of prognosis after a heart attack and sometimes quality of life may be greatly impaired.
Lets look at the primary endpoints we are concerned with using risk in absolute terms.
Nonfatal coronary event: Its pretty clear that incidence of non-fatal cardiac related events are lowered through statin therapy, although that benefit is much greater in the form of high risk secondary care. The 4S study showed an absolute drop in risk of 4.7% when it comes to having a heart attack in those with high LDL and a high risk of re-infarction. CARE showed a drop of 1.8% in patients with CHD that had normal cholesterol ranges. WOSCOPS had a 1.9% drop in primary prevention for high risk patients while AFCAPS/TexCAPS showed a 1.5% drop in non fatal heart attacks. PROSPER investigated the elderly, who are the most negatively affected by a non fatal coronary event, and found just a 1% drop in statin therapy group. The Jupiter trial, which is probably the study that ushered in the most new patients for statin therapy, showed under a percentage point (.45%) drop in risk of non fatal infarction. This low drop is due to the fact that this population is low risk to begin with.
CHD related mortality: Statins appear to reduce CHD related mortality in high risk groups when used as secondary care, in middle aged men in particular. The 4S study once again showed the highest drop in risk, 3.5%, since they were the highest risk patients. Looking at the other secondary care study, CARE, we see a 1.1% drop. Woscops shows a .4% and the AFCAPS/TexCAPS trial demonstrated a .1% drop in the low risk patients for primary care. Prosper was used as justification to put high risk seniors on statin therapy when there was actually a just .9% decrease in death from CHD. (coincidentally there is a .9% increase in death from cancer in the statin group) The great Jupiter trial had 31 deaths in the experiement group and 37 in the control... this was a base of nearly 9000 people in each group. The drop in absolute risk of death from CVD is .07%- not even .1 percent! Jupiter Trial had no endpoint for CHD related mortality, only mortality from the more general CVD.
All cause mortality: Now this is the endpoint we are most concerned with, and it also happens to be the one where statins show the least benefit. 4S showed an absolute drop in risk in all cause mortality of 3.3%. while CARE showed no significant change. I assume since I could not find any hard data one way or the other it was very even and showing very little trending either way. The Woscops study shows a .9% reduction and ACAPS/TexCaps was trending negative, there were 3 more deaths in the statin group. No significant change in PROSPER either (drop of .2%) Jupiter posted a .5% drop (which it reported as a 20% drop in relative risk)
Some things to take note of
High average BMI and unhealthy lifestly of study participants The average BMI of the patients involved in the studies was 26 on the low end and 30 on the high. A BMI of 26-29 is considered overweight and borderline obese and 30 or above is obese. Why is this important? Well some of the known and established risk factors for heart disease are
- Male sex
- Older age
- Race (those of African, Mexican, or Native American heritage have a higher risk)
- Family history of CHD
- Smoking
- Dyslipidemia
- Diabetes
- Hypertension
- High levels of inflammation
- Physical inactivity
- Being overweight
Having a BMI of 26 or higher (lower if you are of Asian decent) greatly increases your risk of hypertension, dyslipidemia, type 2 diabetes, CHD, stroke, chronic inflammation, cancer, osteoarthritis, metabolic syndrome,and fatigue. So not only is CHD itself a risk of being overweight, but many of the risk factors that make up CHD cross over to the overweight population. If we were to select a population with whats considered an average BMI the statin trials would not be effective in reducing relative risks to a level that influences the public and medical community. But in America unfortunately the average BMI is around 27 so for the average population the sample is quite accurate actually. Many people are willing to take drugs that alter their biochemistry on a fundamental level and quite often look to go that route without first exhausting other ways.
In addition to having high BMI a high percentage of study participants have hypertension and tend to drink and smoke more excessively than the average person would be who is taking steps towards getting healthy. A 2004 study found that 90% of the cases of CVD are caused by a modifiable diet and lifestyle.(27) Looking at the risk factors for CHD all but the first 4 are controllable factors. Consider that essentially 100% of people experience some kind of side effects on statins, and very few receive any benefit when it comes to actual mortality rates. Even in cases where CHD mortality goes down, total mortality almost always has no significant change. In essence you are experiencing a lower quality of life, and not functioning optimally and in return you're simply changing the cause of death on the certificate, not the length of life.
Corporate corruption and conflicts of interest: Big Pharmaceutical companies sponsored every single one of the positive statin studies. They are the only ones with the incentives to shell out the cash needed to organize and complete these large and expensive studies. Some are not published or are even stopped before conclusion for lack of results. Even ones that show zero to very little benefits are trumped up and exaggerated since such a large amount of money was spent on the study.The results are presented in terms of relative risk and stats like the number needed to treat (to recieve a benefit), absolute risk, or the cost of treatment to prevent one event are not publicized as these tend to paint a less favorable picture of statin treatment. At best there is going to be some kind of unintentional bias when those organizing the study are being paid by the ones looking for a positive result from the study. At worse the studies my be manipulated and distorted to achieve desired results.
In 2003 a study was published in the British Medical Journal investigating whether funding of drug studies by the pharmaceutical industry is associated with outcomes that are favorable to the funder and whether the methods of trials funded by pharmaceutical companies differ from the methods in trials with other sources of support. 30 studies were included and it was found that studies funded by pharmaceutical companies were less likely to be published (large incentive to not publish unfavorable results), and that studies published were more favorable when coming from the drug companies. There was no difference found in the quality of drug sponsored and independent studies.(28) 75% of the retracted studies in the drug industry are related to scientific misconduct which is a much larger percentage than in general biomedical literature.(29) On top of this it takes an average of 39 months for a study to be retracted so often many people must suffer before a product is recalled recalled (vioxx anyone?) Phizer was fined $2.3 billion in 2009 which was the largest federal drug company settlement in history and Merck and many others have faced very large fines as well for less than ethical business practices.
fda SUCKLING at the tit of big pharma
In 1992 US Congress passed the Prescription Drug User Fee Act (PDUFA), and that was a pivotal moment. The act authorizes the FDA to collect "user fees" from drug companies in order to increase the speed by which it can conduct drug reviews. A standard drug application must now be completed within 12 months of submission, compared to as much as 30 months prior to PDUFA. Priority applications must be completed within six months. Since the FDA began collecting user fees from the very industry it was intended to regulate, approved drugs have become increasingly dangerous with a higher percentage being recalled. 94% of the FDA's proposed budget increase for 2014 come from drug companies, a total of $770 million.(30) The members that make up the NCEP and AHA which are in charge of putting out cholesterol guidelines almost all have major conflicts of interest and make money from statin producing drug companies. If we are to be optimistic and believe there is no blatant corruption or illegal tactics going on, its impossible to believe that a scientist will not be slightly more inclined to have faith in the effectiveness of a drug when they are being paid to speak about how amazing it is and receive large grants and salary for more research. We must disentangle the governing agencies from Big Pharma.
Statistical manipulations: As I've mentioned earlier studies are "fluffed up" to appear more beneficial than they really are. This is done in a couple of different ways. First a high risk population is usually selected for the study to provide a more favorable result. These people will be overweight or obese, be hypertensive, and live an unhealthy lifestyle. They also typically include a much higher percentage of men than women even though the results are of extrapolated to both sexes. Statistical endpoints are also often misguiding. Usually the primary endpoint is a combination of nonfatal myocardial infarction and CHD related mortality. Drug companies are able to claim large drops of relative risk because of the nonfatal myocardial infarction. Non fatal heart attacks will be greater in those not using statins but the difference in CHD related mortality is often not significant. Its combined with nonfatal MI to reach statistical significance. For example the CARE study reported a statistically significant 24% risk reduction (absolute risk reduction of under 5%) in its primary endpoint of non-fatal MI combined with CHD mortality. Many people interpreted this to mean that statins will prevent CHD related death in the form of secondary care to low risk patients even though there was actually no significant change in CHD mortality by itself, just the combined endpoint. Conversely 13 women developed breast cancer in the statin group and only 1 in the control group. If we were to present this is the same terms of relative risk it would be seen as a 1400% increase in the risk of development of breast cancer. Its all in how the numbers are presented.
Statins marginal benefit may come from pleiotropic effects and not the lowering of LDL-c: Statins are thought to have other mechanisms that help reduce the risk of heart disease such as lowering vascular inflammation and stimulating smooth muscle activation. There have been reductions in vascular events and death from CHD in populations that LDL-c has no relation to either like in women and those over 70. They also prevent heart attacks in those with low LDL-c, and it was shown in the large Heart Protection Survey to prevent stroke which is unrelated to cholesterol levels. Studies like J-LIT and CARE show that lowest LDL doesnt translate to lowest rate of mortality from CHD so there is something is going on besides dyslipidemia. It's very likely much of the benefits of statins does not come the LDL lowering mechanism at all. Therefore it makes sense to try to target your health hollistically and not rely on a drug that is designed to lower LDL. You can lower inflammation dramatically though other less aggressive means such as diet or safer medications than statins.
Bottom line: Statins lower LDL-c levels across the board. They also lower the chance of experiencing a heart attack, although cholesterol could be seen as protective since those that do suffer heart attacks are more likely to die when they have low LDL-c levels.(31) They do not significantly lower the mortality rates from CHD or overall mortality except in the form of secondary care for the high risk male. Statins may not only be useless but in fact harmful to the elderly and post menopausal women. Mortality rates tend to trend negative for these groups when taking moderate to high dose statin therapy. Both women and the elderly develop higher rates of cancer than other populations when on statins. The elderly also experience more neurological related side effects such dementia and memory loss, while women tend to be more prone to developing type 2 diabetes. In my opinion the only populations that should even consider statin therapy are those with moderate famililal hypercholestermia, high risk middle aged men with a history of CHD in the form of secondary care, and someone who has recently had a heart attack. The only population that should consider primary prevention is those with the FH genetic defect. For any other group of people to be prescribed statins without first making lifestyle changes should be considered unethical.
Making sense of your cholesterol numbers and lowering risk
So why is LDL-c the target? It's easily manipulated by drugs... As noted in the first part of this Exploring the Epidemic article LDL-c is not the strongest link to risk of CHD. Instead of just looking at total cholesterol and LDL-c use these as indicators of risk.
- HDL/Total Cholesterol- Should be at least 24% and under 10% is high risk of heart disease.
- Triglicerides/HDL- This number should be under 2. Consuming a diet high in carbohydrates and low in saturated fat skews this ratio negatively.
- Fasting insulin- Ideally below 3
- Fasting blood glucose- under 80 mg/dl
- Body fat percentage- Its very important to be under the obesity threshold, for men this is 25% for women this is 35%
So how do we obtain these desired targets? Well diet most definately plays a large role and many people believe a heart healthy diet to be low in fat and high in breads, cereals, grains, and fruits. A diet in which you consume a high percentage of calories from fructose and processed carbohydrates raises your risk for heart disease by promoting metabolic syndrome which is a cluster of health conditions that includes high blood pressure, insulin and leptin resistance, high triglycerides, liver dysfunction, and visceral fat accumulation.
In addition to to having metabolic deficiencies the average American gets inadequate exercise, suffers from chronic stress and sleep deprivation, is exposed to environmental toxins, and has poor gut health. This is the perfect storm for chronic inflammation and disease. A real heart healthy diet would be free of gluten, processed foods of any kind really, GMO's, industrial meats, refined sugar, artificial sweeteners, and trans fats. You should consume a large amount of organic vegetables, healthy sources of saturated fat like grass fed beef, some fermeneted foods, and your food should be very gently cooked with a portion of it raw. Your carbohydrate intake should not make up more than 30% of your total calories, preferably closer to 20% and under 10% if obese or not active and working out.
Along with the above diet recommendations its also very important to exercise regularly. The 2013 metaanalysis listed above showed exercise just as effective as statin medication at lowering cases of CAD. You must make your body work extremely hard for at least 30 minutes, 2-3 times a week. This will entail periods of high intensity work followed by a rest interval. You should also just move more frequently. Walk, bike, take the stairs, park further etc... we are designed to be moving almost constantly and this will get your heart used to sustained low intensity work in addition to the hard workouts. Also if you are following the diet and not eating large amounts of carbs this will speed up the fat burning process as this is the preferred source of energy for low intensity aerobic exercise. Intermittent fasting is very useful in helping mitigate leptin and insulin resistance which are drivers of higher LDL-p and the dangerous small dense forms of LDL-c.
In Conclusion
Statin use is so widespread its almost looked down upon to question their effectiveness or safety. If your doctor blankly recommends statin therapy without first making major lifestyle changes they are not following their Hippocratic oath to first do no harm. They were approved for use because they were shown to lower LDL-c and LDL-c was known to be loosely correlated with CHD most of the time. However it is clear that LDL-c is not the cause of CHD yet millions are prescribed a drug to target it. The 1984 LRC-CPPT study was the big push that would enable statins to become a $30 billion dollar commodity. This study was very flawed since all patients had FH, and the results were greatly exaggerated. The FDA, NIH, AHA, NCEP, and other organizations all have had major incentives for statin therapy to be widespread. Beginning in the early 90's drug companies sought to get larger market shares and recommended statins for much more widespread use going from being prescribed to those with specific genetic defects and the very high risk to 1 in 4 Americans, mainly for primary care. Any marginal benefit was exaggerated and the negative sides are often downplayed since they are often considered a sign of aging, such as degenerative muscle pain and memory loss. Statins make it difficult to workout and recover and they speed up the aging process. Exercise and lifestyle modifications are just as effective at reducing CHD related mortality as statins and you aren't dealing with sides or messing with your blood sugar increasing your risk of diabetes in the process. We should not be altering one of the most fundamental processes in our body, the production of cholesterol. It's time we stop relying on pills to take care of the symptoms and finally address the root cause.
Reccommened further reading
How statin drugs really lower cholesterol & kill you one cell at a time- A review and summary of the book of the same title. Talks about the mechanism of lowering cholesterol and corporate influences.
How Statins Really Work Explains Why They Don't Really Work- Dr. Seneff from MIT has put together a very detailed and through paper on how statins work and their side effects.
Cholesterol is NOT the Cause of Heart Disease- Very good article detailing how we blame cholesterol for heart disease and explores the other pieces to the complex puzzle.
The Diabetes Dilemma for Statin Users- Article from the New York Times that was published after the FDA started to require drug companies to put warnings for diabetes on statin labels.
Statins Are the Greatest Medical Fraud of All Time: Study Reports- Article exploring the 2013 study and emphasizing the major points
$tatin Nation- Great in depth documentary about the over prescription and overuse of statins.
Sources without direct link
1- . Vila, A. Rebollo, G.S. AÄ‘alsteisson, M. Alegret, M. Merlos, N. Roglans, and J.C. Laguna, "Reduction of liver fructokinase expression and improved hepatic inflammation and metabolism in liquid fructose–fed rats after atorvastatin treatment," Toxicology and Applied Pharmacology 251, 32–40, 2011.